OVERVIEW
Crohn's disease is a chronic inflammatory disease of unknown origin potentially affecting all parts of the gastrointestinal tract. While medical management of the disease is often the first choice, surgery may be indicated for specific reasons. Crohn's disease most commonly affects older adolescents and adults. It is extremely important to make an accurate diagnosis because Crohn's disease is one of several types of inflammatory bowel disease. Patients with Crohn’s disease can have the same symptoms as those with other types of inflammatory bowel diseases such as ulcerative colitis.
WHAT IS CROHN’S DISEASE
Patients with Crohn’s disease experience lifelong inflammation of the gastrointestinal tract that always involves the innermost inner lining of the gastrointestinal wall, known as the mucosa, though it can extend to the deeper layers of the wall. The most common area of involvement is the point where the small bowel joins the large bowel called the ileocolic region. However, Crohn's disease can occur at any point in the gastrointestinal tract from the mouth to the anus and can affect one or more areas. There is no way to predict who will develop this disease or when the disease may appear. It is a chronic condition that can appear at any time, can go into remission without explanation, and can recur without apparent cause. Unlike ulcerative colitis, there is no cure for Crohn's disease. However, medical and surgical management of Crohn’s disease often provides patients with long periods of clinical remission.
 Figure 1. Diagram showing Crohn’s disease affecting the last part of the small bowel (ileum) and/or the large bowel (colon)
Figure 1. Diagram showing Crohn’s disease affecting the last part of the small bowel (ileum) and/or the large bowel (colon)
WHO IS AT RISK FOR CROHN’S DISEASE?
Crohn’s disease can affect anyone at any age, but most often appears in the third decade of life and there has been an observed second peak in the sixth or seventh decade. Both men and women are affected equally by this disease. A family history of Crohn's disease or inflammatory bowel disease slightly increases a person’s risk of developing Crohn's disease. Smokers are at increased risk for developing the disease.
WHAT CAUSES CROHN’S DISEASE?
The exact cause of the disease is not known. Current research is focused on abnormalities in the body's immune system and on bacterial infection. At this time, it seems most likely that Crohn’s disease is a form of autoimmune disease, where the patient’s own immune system attacks the intestinal tract, causing inflammation. This assumption is supported by evidence that symptoms are relieved when medications are used that suppress the immune system. Crohn’s disease is not contagious.
WHAT ARE THE SYMPTOMS OF CROHN’S DISEASE?
Most commonly, Crohn’s disease appears as abdominal disease (affecting the small or large intestine), as anorectal disease (affecting the anus and/or rectum), or as both. Onset and symptoms vary widely and may include intestinal cramping, pain, persistent diarrhea or constipation, bleeding with bowel movements, fever, fatigue, and weight loss. Not all of the symptoms will appear in every patient. Occasionally, the onset of Crohn's disease is sudden and severe; the patient quickly becomes very sick, and surgery is required immediately.
Some patients with Crohn’s disease develop a fistula, which is an abnormal passageway between the bowel and other body parts including bowel loops, other organs, and/or skin surfaces. Fistulas can form between loops of bowel, between bowel and bladder, between bowel and vagina, or between bowel and skin. The anorectal symptoms include anal pain, and/or drainage from the perianal area. These symptoms may also be caused by a persistent perianal abscess (pocket of infection) or anal fissure (painful cleft or groove).
WHAT IS THE EVALUATION OF CROHN’S DISEASE?
The initial work-up of the patient includes taking a thorough medical history and physical examination followed by laboratory testing, examination of the inside of the bowel using instruments with a flexible lighted camera (colonoscopy), and radiology studies.
The laboratory tests may include basic blood work that can assess for inflammation and other clues about the diagnosis. In addition to blood work, an examination of the inside of the bowel is usually required because this is the most accurate way to determine the extent of the disease. The most common of these examinations is a colonoscopy. It is a procedure used to evaluate the inner lining of the colon and rectum as well as the distal-most portion of the small intestine. A colonoscope is a long, thin, tube-like, flexible instrument placed through the anus that provides magnified views of a patient’s large intestine (colon and rectum) and sometimes the small intestine. The colonoscope is commonly used to detect a variety of colon and rectal problems as well as to remove colon polyps and to screen for colon cancer. The procedure is frequently performed in an outpatient setting with minimal discomfort and inconvenience.
The finding of inflamed mucosa, stricture, or the opening of a fistula tract will help confirm the diagnosis of Crohn's disease and will help determine the extent of bowel involvement. These findings will be used to determine a surgical plan if surgery is being considered.
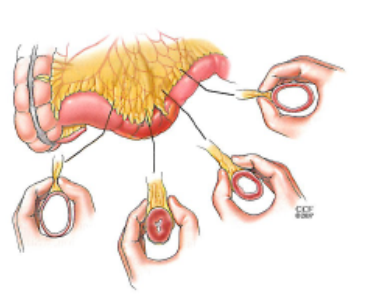
Figure 2. Figure showing the narrow luminal opening due to thickening of small bowel wall from Crohn’s disease
Radiographic studies may include a CT or an MRI scan of the abdomen and pelvis to evaluate for inflammation or narrowing of the bowel, intraabdominal abscesses (pockets of infection), or a fistula connection between bowel and other structures. Usually, this study requires the patient to drink a solution containing contrast material so that these abnormalities can be more clearly visualized. To differentiate chronic versus recent inflammation, your physician may sometimes order additional tests to show the inflammation and affected areas in greater detail.
WHAT ARE THE TREATMENT OPTIONS FOR CROHN’S DISEASE?
Treatment for Crohn’s disease is broadly categorized as medical or surgical in nature. It is important to note that there is currently no identified cure for Crohn’s disease. Medical management is aimed at achieving and maintaining a non-inflamed state and attempting to prevent recurrent disease. Surgical therapy is indicated for managing the complications of Crohn’s disease (such as obstruction, fistula, bleeding, and perforation). Surgical removal of the segment(s) of intestine involved with Crohn’s disease does not cure the disease. Removal of the segment(s) addresses the immediate problem but the disease often returns in areas previously not involved, often just upstream to the area where two previously healthy pieces of intestine are joined.
Once the diagnosis is made, medical management usually is the first choice for treatment unless, as mentioned above, the patient's condition requires an emergency operation. In medical management, several treatment plans are available for initial therapy, for maintenance therapy, and to prevent recurrence. These medical treatment options are often managed by the patient's gastroenterologist (a physician who specializes in the non-operative management of diseases of the intestine). Other medications may also be prescribed depending on your history, age, general health, and specific disease process. Dietary modifications might also be recommended. If medical management is unable to relieve the pain, obstruction or fistula formation, surgery then becomes an option to improve the patient's health.
SURGICAL TREATMENT
- Surgery for Crohn's disease may either be scheduled (elective surgery) or done in emergency. Emergency surgery is performed for patients who have developed conditions requiring treatment within a few hours of coming to the hospital. Usually, these patients have either a bowel perforation (a hole in the bowel resulting in fecal matter leaking into the abdomen) or a complete obstruction (blockage) of the bowel. Both of these conditions can be life-threatening. Occasionally, a patient will require emergency surgery for a perirectal abscess (pocket of infection by the anus) to drain the fluid collection in order to prevent further damage or spread of infection.
- Elective surgery for Crohn’s disease might be performed for patients who have poor quality of life because of Crohn’s disease despite medical treatment. This also applies to patients that no longer respond to medical therapy,or cannot comply with long term medication or deal with significant side-effects of medical treatment.
If surgery is indicated, the procedure will either be abdominal surgery or anorectal surgery. Abdominal surgery addresses the entire abdomen, while anorectal surgery is restricted to the immediate anal area. Abdominal surgery can be done as a traditional open surgical procedure or as a laparoscopic or robotic minimally invasive procedure using small incisions and a camera. Your surgeon will decide between an open or minimally invasive procedure based on the extent of your disease and on which of these procedures would be safest with your history and general health. Whether done as an open or minimally invasive procedure, abdominal surgery is performed to address a section of diseased bowel.
Most common types of surgery for Crohn’s Disease:
- Ileocolic resection: removal of the end of the small bowel and the beginning of the large bowel
- Stricturoplasty: procedure to relieve bowel strictures.
- Small (enterectomy) and/or large bowel resection (colectomy or proctocolectomy) : resection of the diseased part of the bowel, and joining the healthy ends together (anastomosis)
- Fistula resection: Resection of the abnormal passageway between bowel and other structures
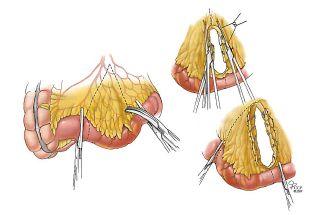
Figure 3. Diagram showing the removal of portion of thickened small bowel with primary reconnection.


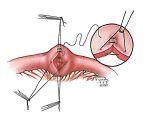
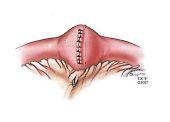
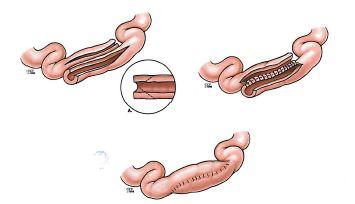
Figure 4. Diagram showing two types of stricturoplasty. The narrowed portion of the bowel is opened and reconnected without resection to preserve the bowel length.
These are performed with the intent to preserve as much bowel length as possible to improve the patient's prospect for more normal digestive function. Because there is no cure for Crohn’s disease and recurrence is common, your surgeon will want to preserve as much intestinal length as possible with each surgery. There is a high chance of recurrence depending on the severity of the disease.
Following removal of a portion of the bowel, it is not always possible or prudent to reconnect the remaining bowel into a continuous length. When this is the case, a patient may need an ostomy to pass stool. An ostomy is a surgically created opening between the small or large intestine and the surface of the abdominal wall. The part of the bowel that is seen on the abdomen surface is called a stoma. Ostomies may be intended to be permanent or temporary, depending on the particular circumstances.
Anorectal surgery for Crohn’s disease is most commonly performed to drain a perianal abscess. During the procedure, the infected cavity is opened, and the fluid drained out. In cases where the infection process is still active and fluid is still being formed, a fistula (connection to the diseased anus or rectum draining outside next to the anus) may be present. Your surgeon may place a piece of suture or thin rubber band-like material as a loop through the fistula tract, commonly called a seton. Placing a seton promotes controlled drainage and helps avoid undrained abscess pockets from reforming. The seton will be left in place until medical management is able to keep the drainage under control (normally weeks), at which point the surgeon can consider removing it.
Anorectal surgery is also performed to correct a fistula (an abnormal passageway between the bowel and nearby organs or between the bowel and skin). In the setting of one or more significant anal fistulas, patients are occasionally recommended to undergo ostomy creation to divert the stool away from the anal fistulas until medical management can become effective and the wounds have completely healed. The ostomy can often be reversed once the wounds have healed, but this will depend upon the patient's overall general health and the progress of their Crohn's disease.
WHAT DO I NEED TO DO AFTER SURGERY?
Your gastroenterologist will want to re-establish care very quickly after surgery. At that follow-up appointment, your gastroenterologist may introduce a medication regimen to control the disease and prevent recurrence.
Patients with inflammatory bowel disease (Crohn’s disease or ulcerative colitis) are at increased risk for developing colon and rectal cancers. In patients with longstanding colonic Crohn’s disease, the increased risk for developing colon or rectal cancer can be up to 2-3 fold. The guidelines currently in use recommend that these patients undergo an initial screening colonoscopy within eight years after the onset of symptoms, followed by surveillance colonoscopy. Time to surveillance is depending on the findings of the index (initial screening) colonoscopy.
HOW CAN I REDUCE RECURRENCE?
Recurrence is often seen in patients who continue to smoke. It is also common in patients who stop their medications to treat their Crohn’s disease either because of their inability to afford the medications or their refusal to continue with the lifelong treatment. Crohn's disease is a chronic, lifelong condition that requires continuous attention to control.
QUESTIONS FOR YOUR SURGEON
-
When do I need surgery?
-
What are my options for surgery?
-
What operative approach will be used (open or minimally invasive surgery)?
-
What is the likelihood of my needing a stoma/ostomy with this surgery?
-
What can I expect after surgery?
-
When do I need a repeat colonoscopy?
-
How will my pain be addressed after surgery?
-
What could happen if I didn’t want any surgical treatment?
WHAT IS A COLON AND RECTAL SURGEON?
Colon and rectal surgeons are experts in the surgical and non-surgical treatment of diseases of the colon, rectum, and anus. They have completed advanced surgical training in the treatment of these diseases, as well as full general surgery training. Board-certified colon and rectal surgeons complete residencies in general surgery and colon and rectal surgery, and pass intensive examinations conducted by the American Board of Surgery and the American Board of Colon and Rectal Surgery. They are well versed in the treatment of both benign and malignant diseases of the colon, rectum, and anus and are able to perform routine screening examinations and surgically treat conditions, if indicated to do so.
DISCLAIMER
The American Society of Colon and Rectal Surgeons is dedicated to ensuring high-quality patient care by advancing the science, prevention and management of disorders and diseases of the colon, rectum and anus. These brochures are inclusive but not prescriptive. Their purpose is to provide information on diseases and processes, rather than dictate a specific form of treatment. They are intended for the use of all practitioners, health care workers and patients who desire information about the management of the conditions addressed. It should be recognized that these brochures should not be deemed inclusive of all proper methods of care or exclusive of methods of care reasonably directed to obtain the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all the circumstances presented by the individual patient.
ASCRS committee members review and update information for accuracy. We believe content is medically accurate at the time it was produced.
CITATIONS
Bickston, S.J. and Bloomfeld, R. S. Handbook of Inflammatory Bowel Disease.Lippincott Williams & Wilkins, Baltimore, MD; 2010 Strong, S.A. Chapter 30, “Crohn’s Disease: Surgical Management” .
Chapter in Beck, D. E., Roberts, P.L., Saclarides, T.J., Senagore, A.J., Stamos, M. D., Wexner, S.D.. Eds. ASCRS Textbook of Colon and Rectal Surgery, 2nd Edition. Springer, New York, NY; 2011
ASCRS website, 2011 Core Subjects; Efron J “Crohn’s Disease”
Strong, S. A., Koltun, W. A., Hyman, N. H., Buie, W. D.; Standards Practice Task Force, American Society of Colon and Rectal Surgeons. Practice Parameters for the Surgical Management of Crohn’s Disease (Revised 2007). Dis Colon Rectum.2007;50(11):1735-1746.
Lightner AL, Vogel JD, Carmichael JC, Keller DS, Shah SA, Mahadevan U, Kane SV, Paquette IM, Steele SR, Feingold DL. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Surgical Management of Crohn's Disease. Dis Colon Rectum. 2020 Aug;63(8):1028-1052. doi: 10.1097/DCR.0000000000001716. PMID: 32692069.
ACKNOWLEDGEMENT:
ASCRS thanks Sanda A. Tan, MD, PhD, for her assistance with the development of this educational brochure.